Vaginal cysts are uncommon, their prevalence is unclear but it is estimated to be close to 1%. They are usually asymptomatic and an incidental finding during gynecological examination. Some patients may present with vaginal discomfort, perineal pressure, or a bulging vaginal mass. In some cases, it may produce dyspareunia, vaginal spotting, or low urinary track symptoms. When these cysts present, patients are usually at the third or fourth decade of life.
They are classified based on origin and histologyin four different types:
A) Mullerian cyst paramesonephric 30 %
B) Bartholin duct cyst – 27, 5%
C) Epidermal inclusion cyst squamous – 25%
D)Gartner duct cyst – mesonephric Endometroid cyst and unclassified variety – 17, 5%
The origin of these cysts is not clearly understood, but some of the theories described in the literature link these masses with aberrant embryogenesis, with ectodermal cells misplaced during cellular differentiation; it could also be caused trauma, injury or pressure to an area transplants epidermal cells into the tissue.
Epidermoid cysts are essentially benign and slow growing lesions that arise from implantation of epidermis into the dermal layer of skin or as in this case, the vagina. Vaginal trauma like an episiotomy, vaginal tears during delivery, and iatrogenic implantation of epidermal fragments via surgical tools can explain this rare location of an epidermal vaginal cyst.
The most common sites where they can be found are in hairy areas. With 90% of lesions found in the scalp, followed by other sites include trunk, neck, face, arms and legs and lastly and less frequent at the genital area.
These vaginal inclusion cysts are generally small and can be found at the lower end of the vagina, usually on the posterior wall. Near the fornix, they arise from epithelial inclusion below the surface of the vagina because of fragments of mucosa resulted from perineal tears or from an improper surgical technique during repair of the perineum, after an episiotomy.
There are other very rare presentations of epidermal cysts described in some women as in the gastrointestinal tract (colon), clitoris and retroperitoneum as an adnexal tumor. Some of the largest pelvic cysts have measured up to 17.8 × 13.18 cm reported in 2010 (9) followed by a 15 × 10 cm cyst, reported in 2012.
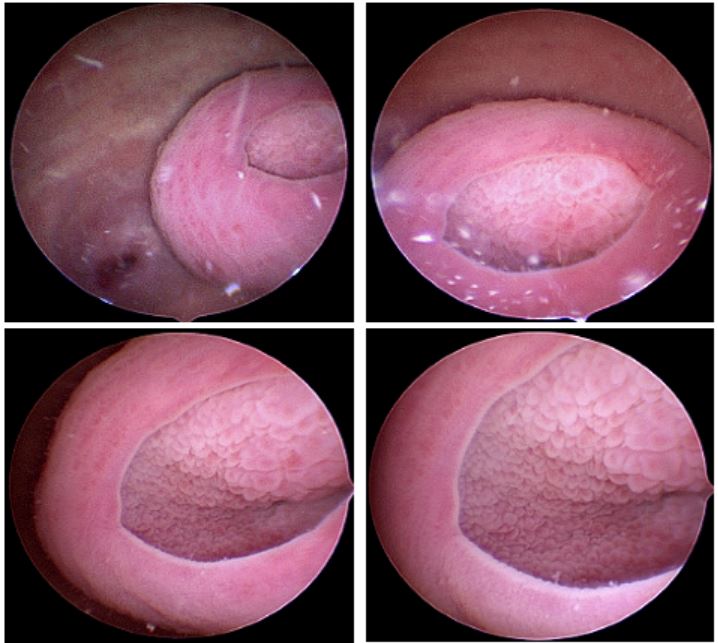
In this case, we consider the patient’s spontaneous vaginal delivery and episiotomy repair with vaginal instrumentation as the only contributory factor to the formation of the cyst. The patient denies vaginal tears or forceps. The use of vaginoscopy allowed us to have an endoscopic close view of this rare pathology, even though it is not the standard of care to use it in cases like this.